Facts about the Chikungunya
BackFACTS
- Chikungunya (chik'-en-GUN-yah), also called chikungunya virus disease or chikungunya fever, is a viral illness that is spread by the bite of infected mosquitoes.
- The disease resembles dengue fever, and is characterized by severe, sometimes persistent, joint pain (arthiritis), as well as fever and rash. It is rarely life-threatening.
- Chikungunya occurs in Africa, India and Southeast Asia. It is primarily found in urban /peri-urban areas.
- There is no specific treatment for chikungunya.
- Prevention centers on avoiding mosquito bites in areas where chikungunya virus may be present, and by eliminating mosquito breeding sites.
1. What is Chikungunya?
Chikungunya (also known as chikungunya virus disease or chikungunya fever) is a debilitating, but non-fatal, viral illness that is spread by the bite of infected mosquitoes. It resembles dengue fever.
2. Which are the states affected by Chikungunya?
In 2006 Chikungunya re-emerged in the Country. Almost all States are affected by Chikungunya.
3. When was chikungunya epidemic outbreak occurred in the past?
In India a major epidemic of Chikungunya fever was reported during the last millennium viz.; 1963 (Kolkata), 1965 (Pondicherry and Chennai in Tamil Nadu, Rajahmundry, Visakhapatnam, and Kakinada in Andhra Pradesh; Sagar in Madhya Pradesh; and Nagpur in Maharashtra) and 1973, (Barsi in Maharashtra). Thereafter, sporadic cases also continued to be recorded especially in Maharashtra state during 1983 and 2000.
4. What is the infectious agent that causes Chikungunya?
Chikungunya is caused by the chikungunya virus, which is classified in the family Togaviridae, genus Alphavirus.
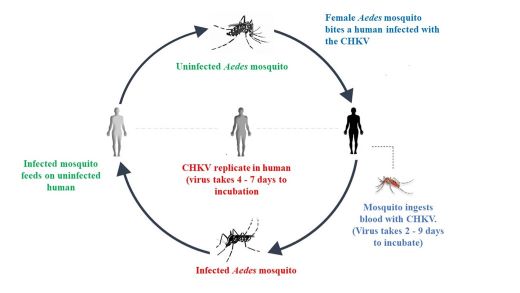
5.How is Chikungunya spread?
Chikungunya is spread by the bite of an Aedes mosquito, primarily Aedes aegypti. Humans are thought to be the major source, or reservoir, of chikungunya virus for mosquitoes. Therefore, the mosquito usually transmits the disease by biting an infected person and then biting someone else. An infected person cannot spread the infection directly to other persons (i.e. it is not a contagious disease). Aedes aegypti mosquitoes bite during the day time.
TRANSMISSION CYCLE
6. Where is chikungunya found?
Chikungunya occurs mainly in Africa and Southeast Asia. It is sustained by the human-mosquito-human transmission cycle
7. What are the symptoms of chikungunya?
Chikungunya usually starts suddenly with fever, chills, headache, nausea, vomiting, joint pain, and rash. In Swahili, "chikungunya" means "that which contorts or bends up". This refers to the contorted (or stooped) posture of patients who are afflicted with the severe joint pain (arthritis) which is the most common feature of the disease. Frequently, the infection causes no symptoms, especially in children. While recovery from chikungunya is the expected outcome, convalescence can be prolonged and persistent joint pain may require analgesic (pain medication) and long-term anti-inflammatory therapy. Infection appears to confer lasting immunity.
8. How soon after exposure do symptoms appear?
The time between the bite of a mosquito carrying chikungunya virus and the start of symptoms ranges from 4 to 7 days.
9.How is chikungunya diagnosed?
Chikungunya is diagnosed by blood tests (ELISA). Since the clinical appearance of both chikungunya and dengue are similar, laboratory confirmation is important especially in areas where dengue is present. These tests are conducting by identified SSHs (783) & ARLs (17) by IgM kits supplied by NIV to the identified SSHs & ARLs.
10. Who is at risk for chikungunya?
Anyone who is bitten by an infected mosquito can get chikungunya.
11.What is the treatment for chikungunya?
There is no specific treatment for chikungunya.
NCVBDC recommends to follow Clinical Management of Chikungunya Fever – 2016 available at https://ncvbdc.mohfw.gov.in/WriteReadData/l892s/77728737401531912419.pdf
12. How common is chikungunya globally?
The first recognized outbreak occurred in East Africa in 1952-1953. Soon thereafter epidemics were noted in the Philippines (1954,1956 & 1968), Thailand, Cambodia, Vietnam, India, Burma, and Sri Lanka. Since 2003, there have been outbreaks in the islands of the Pacific Ocean, including Madagascar, Comoros, Mauritius , and Reunion Island . In January 2006, in an epidemic that is currently ongoing in Reunion Island, over ten thousand cases have been reported. It is suspected that many cases of chikungunya are either misdiagnosed or go unreported.
13.How can chikungunya be prevented?
There is neither chikungunya virus vaccine nor drugs are available to cure the infection. Prevention, therefore, centres on avoiding mosquito bites. Eliminating mosquito breeding sites is another key prevention measure. To prevent mosquito bites, do the following:
- Use mosquito repellents on skin and clothing
- When indoors, stay in well-screened areas. Use bed nets if sleeping in areas that are not screened or air-conditioned.
- When working outdoors during day times, wear long-sleeved shirts and long pants to avoid mosquito bite.
14.How can Aedes mosquito breeding be controlled?
(a) Source reduction Method
- By elimination of all potential vector breeding places near the domestic or peri-domestic areas.
- Not allowing the storage of water for more than a week. This could be achieved by emptying and drying the water containers once in a week.
- Straining of the stored water by using a clean cloth once a week to remove the mosquito larvae from the water and the water can be reused. The sieved cloth should be dried in the sun to kill immature stages of mosquitoes.
(b) Use of larvicides
- Where the water cannot be removed but used for cattle or other purposes, Temephos can be used once a week at a dose of 1 ppm (parts per million).
- Pyrethrum extract (0.1% ready-to-use emulsion) can be sprayed in rooms (not outside) to kill the adult mosquitoes hiding in the house.
(c) Biological control
- Like introduction of larvivorous fish, namely Gambusia and Guppy in water tanks and other water sources.
For details follow Integrated Vector Management 2022. Link is https://ncvbdc.mohfw.gov.in/Doc/Guidelines/Manual-Integrated-Vector-Management-2022.pdf